Spirometry: how it works. Discover the science behind it.
Kuopio, Finland
February 19, 2024
Spirometry stands as a cornerstone in the diagnosis and management of pulmonary diseases, offering a window into the functioning of the lungs that is both non-invasive and straightforward. This essential pulmonary function test measures how much and how quickly a person can move air in and out of their lungs. It is pivotal for detecting, assessing, and monitoring respiratory conditions, making it a staple in both clinical and research settings. The simplicity of the procedure belies the critical insights it provides into respiratory health.
The Science behind spirometry
At its core, spirometry is a test of lung function that revolves around the measurement of air volume and flow rates during inspiration and expiration, as illustrated in the accompanying spirogram:
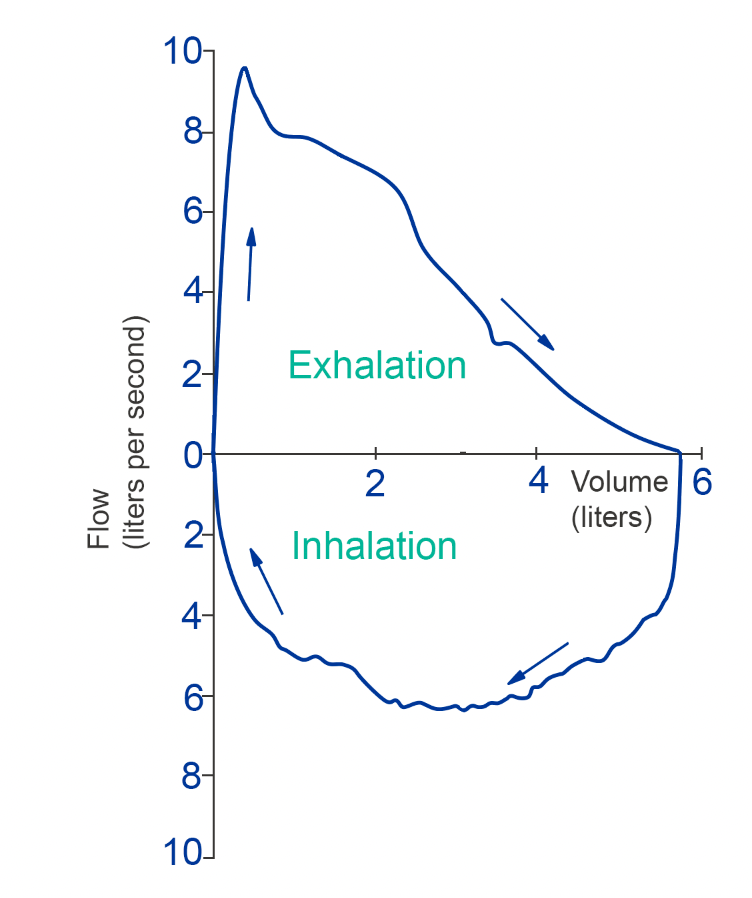
This graph visually represents these parameters: the X-axis shows the volume of air the lungs can hold or expel, and the Y-axis displays the flow rate, or the speed at which air is inhaled or exhaled. The resultant curve offers a snapshot of lung capacity and respiratory strength, which are crucial for diagnosing and understanding the severity of pulmonary conditions. By examining the height and width of the curve — indicative of the flow rate and volume, respectively — clinicians can identify characteristic patterns that disease states may present.
Spirometry system
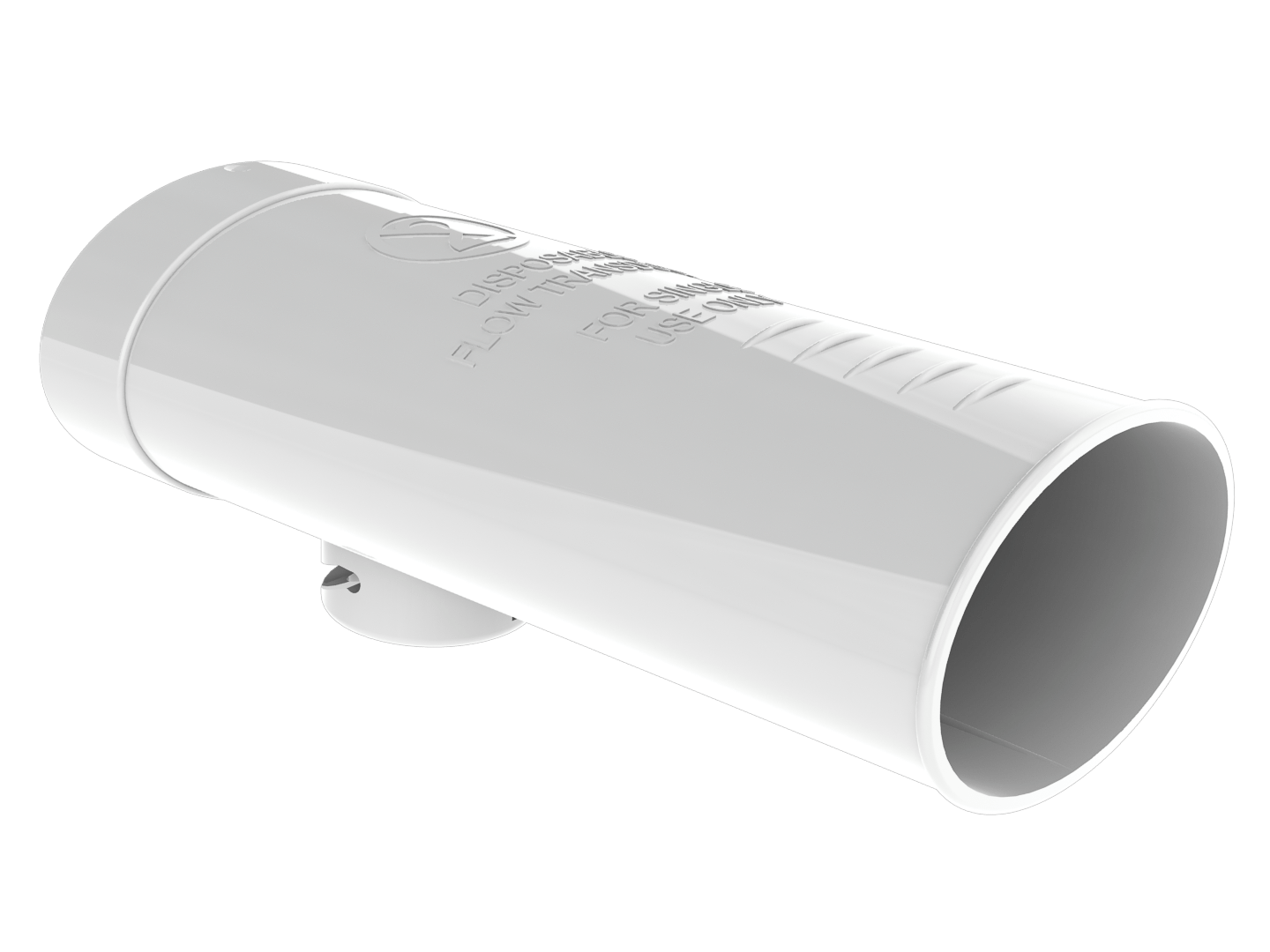
A spirometry test is a symphony of precision, where every component plays a vital role. The flow transducer (in our case – disposable “SpiroSafe flow transducer”) is the point of contact for the patient, designed for comfort and to ensure a proper seal during the test. When a patient exhales, the force of their breath doesn’t send air directly into the spirometer. Instead, the pressure generated is captured within the flow transducer and transmitted through a pressure tube to the sensor housed within the spirometer (for example, Medikro Pro – our bestseller across the globe). This sensor is the heart of the system, translating the analog pressure variations into a digital signal that can be analyzed by specialized software.
Through this process, the volume and flow of air are meticulously measured, allowing for accurate assessments without the risk of cross-contamination between patients, thanks to the use of disposable flow transducers. Medikro’s commitment to innovative design ensures that each test is not only precise but also hygienic and safe for both patients and healthcare providers.
Spirometry procedure
Undergoing a spirometry test involves a series of steps to ensure accurate and reliable results. Patients are usually seated comfortably and use a flow transducer that is connected to the spirometer device for the test. They are guided to take a deep breath to fully inflate their lungs with air, followed by a rapid and forceful exhalation into the flow transducer.
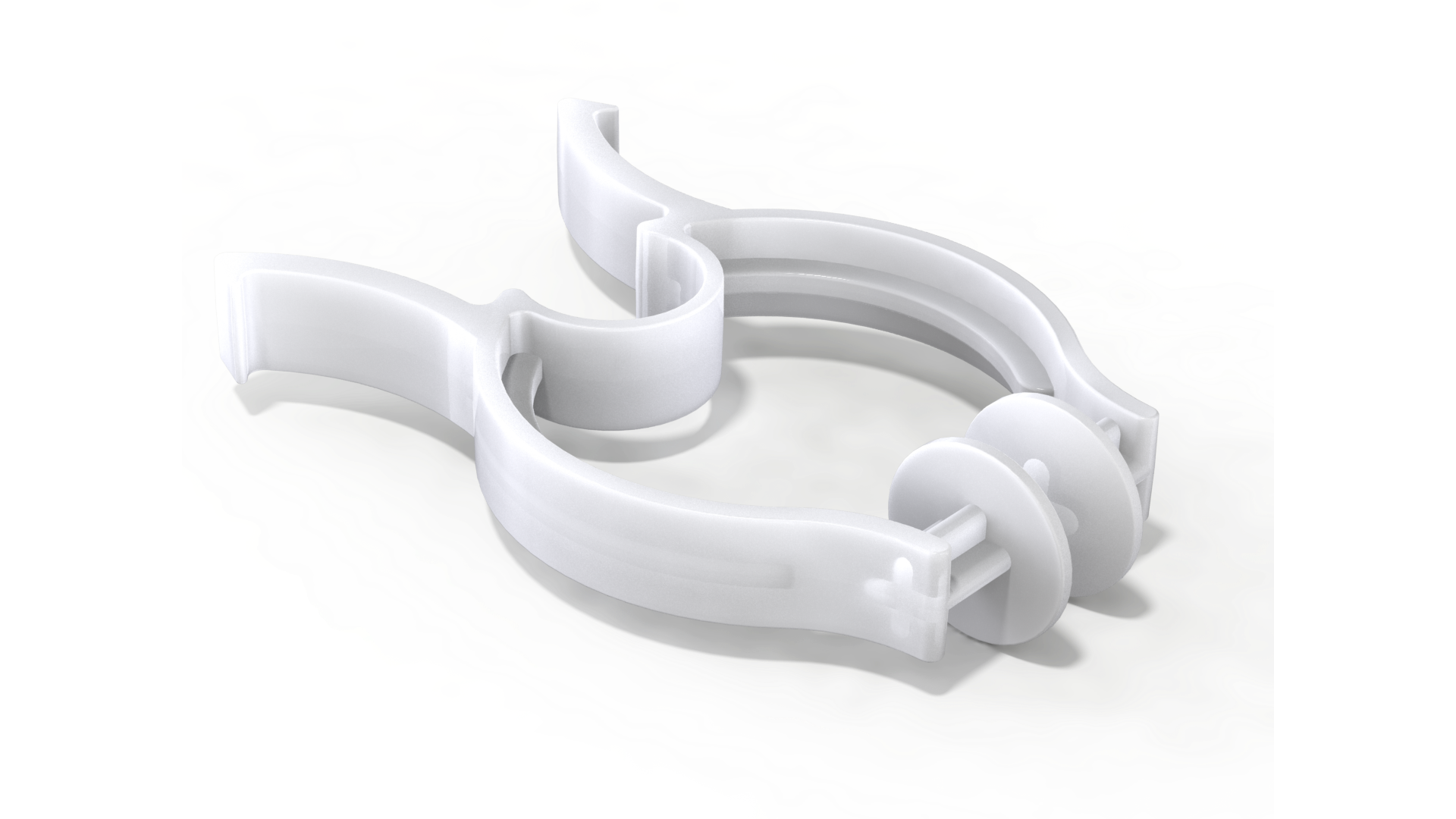
To ensure the accuracy of the test, patients are advised to wear a nose clip during the procedure. This precaution helps to prevent air from escaping through the nostrils, which could otherwise result in a misleading indication of reduced lung volume. It’s crucial that all the air is directed through the disposable flow transducer to capture a precise measurement of lung function. This process may be repeated several times to ensure consistency in the readings.
Correct technique is crucial for obtaining valid results. Patients must ensure a tight seal around the flow transducer and avoid leaks during the test. The procedure is supervised by a healthcare professional who can provide guidance and ensure the technique is correctly performed.
Types of measurements
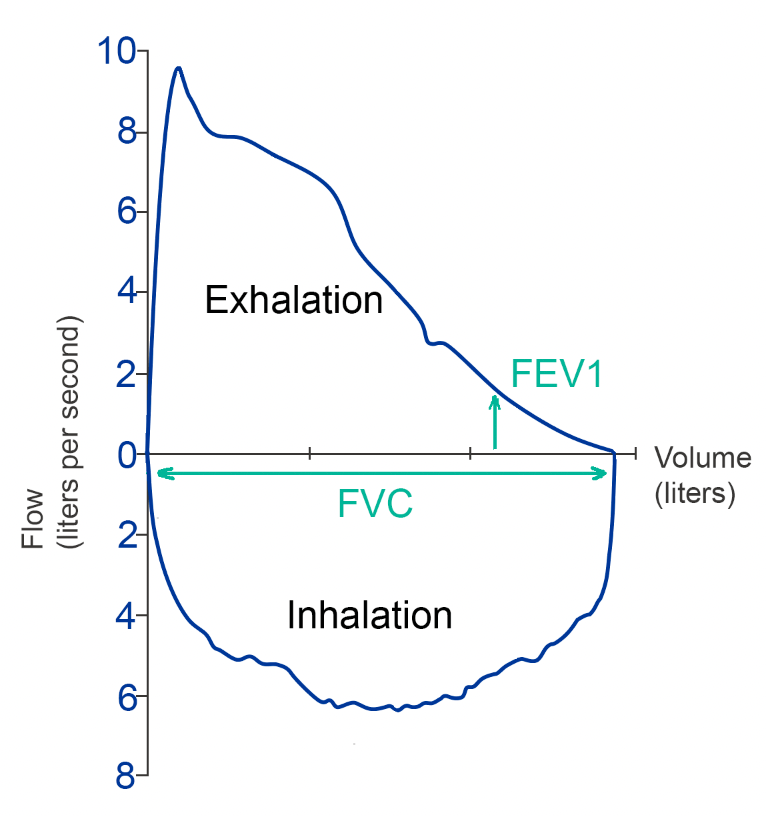
The primary measurements obtained during spirometry include Forced Vital Capacity (FVC) and Forced Expiratory Volume in one second (FEV1). FVC measures the maximum amount of air a person can forcefully exhale after a deep breath, indicating the overall capacity of the lungs. FEV1 quantifies the amount of air expelled in the first second of the FVC maneuver, reflecting the speed of air flow and potential obstruction in the airways. The ratio of FEV1 to FVC is a critical metric used to diagnose and assess the severity of obstructive lung diseases.
Applications
Spirometry is indispensable in the diagnosis and management of a wide array of respiratory conditions. It is particularly crucial in the assessment of chronic obstructive pulmonary disease (COPD) 1 and asthma, where it aids in determining the severity of airway obstruction and monitoring the response to treatment 2. Furthermore, spirometry can help in the evaluation of restrictive lung diseases, such as pulmonary fibrosis, by measuring reduced lung volumes. Its utility extends beyond diagnosis; spirometry is also used in preoperative assessments, occupational health, and in monitoring lung health in patients with chronic conditions 3.
Conclusion
Spirometry is a fundamental tool in the arsenal of respiratory health assessment, providing vital information on lung function that is essential for diagnosing, monitoring, and managing pulmonary diseases. Its simplicity, coupled with the depth of insight it offers, makes it an invaluable procedure in healthcare.
Understanding how spirometry works, from the underlying scientific principles to its practical application, helps to promote its role in advancing respiratory health and patient care. Medikro leads in this area, drives innovation and sets standards in the diagnostics of respiratory diseases. Our commitment to improving the quality and availability of spirometry testing is a commitment we live up to every day. “Spirometry simplified” isn’t just our motto – it’s our promise as we continue to be recognized globally for our contributions to healthcare.
Read more:
Advancing respiratory care in Murcia with Medikro’s spirometry technology
References
1. A systematic review for a clinical practice guideline on the management of stable chronic obstructive pulmonary disease (COPD) underscores the role of spirometry in guiding treatment decisions, highlighting the effectiveness of inhaled therapies and the need for spirometric testing in clinical practice
Wilt, T., Niewoehner, D., MacDonald, R., & Kane, R. (2007). Management of Stable Chronic Obstructive Pulmonary Disease: A Systematic Review for a Clinical Practice Guideline. Annals of Internal Medicine, 147, 639-653. https://doi.org/10.1097/01.HCR.0000314212.63041.42.
2. Clinical and Spirometric Control and Inflammatory Process Assessment: Spirometry aids in the comprehensive assessment of asthma by quantifying the degree of airway obstruction. This is essential for diagnosing asthma and is recommended alongside clinical assessment and the evaluation of the inflammatory process. Despite the utility of clinical assessments and quality of life evaluations, patients may still exhibit airway inflammation and obstruction, which spirometry can help to identify. This emphasizes the need for a multifaceted approach to asthma management, where spirometry plays a pivotal role.
Andrade, C., Chatkin, J., & Camargos, P. (2010). Assessing clinical and spirometric control and the intensity of the inflammatory process in asthma.. Jornal de pediatria, 86 2, 93-100. https://doi.org/10.2223/JPED.1964.
3. The American Thoracic Society’s technical standards for spirometry in the occupational setting provide recommendations for the performance and interpretation of workplace spirometry, underlining its importance in monitoring lung health in relation to workplace exposures
Redlich, C., Tarlo, S., Hankinson, J., Townsend, M., Eschenbacher, W., Essen, S., Sigsgaard, T., & Weissman, D. (2014). Official American Thoracic Society technical standards: spirometry in the occupational setting.. American journal of respiratory and critical care medicine, 189 8, 983-93 . https://doi.org/10.1164/rccm.201402-0337ST.